Celebrating Integrated Neighbourhood Working in Nottingham City
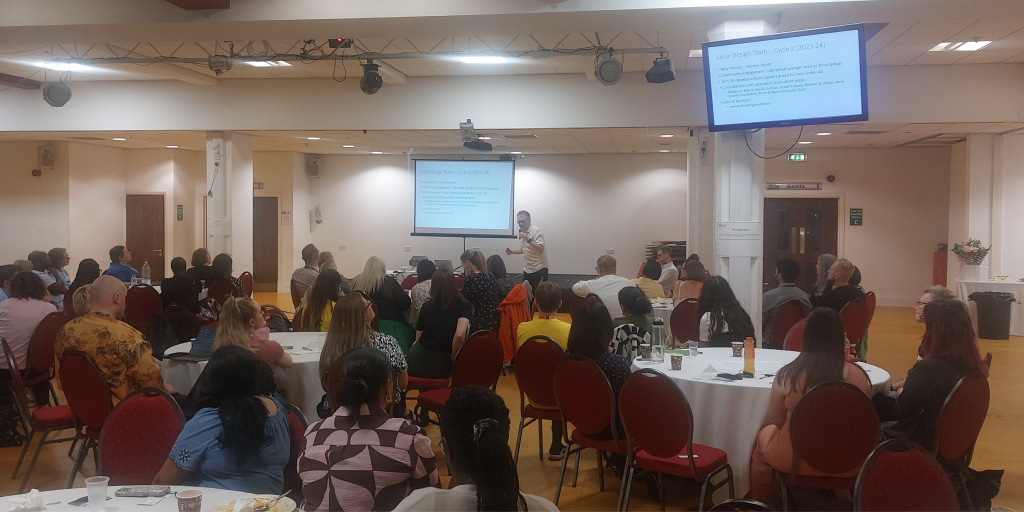
On 2 July 2025, partners from across Nottingham City came together to celebrate the innovative work happening in within integrated neighbourhood working.
As highlighted in the NHS 10 Year Plan (released the following day), neighbourhood working is essential to shifting care from hospitals into communities, with a greater focus on prevention. This event, held during Co-Production Week, offered a valuable platform for teams to share insights, challenges, and successes in delivering joined-up care.
Dr Andy Foster (GP and Nottingham City PBP Deputy Clinical Lead) opened the event by emphasising the urgent need for collaboration, citing the 13-year life expectancy gap between the City’s wealthiest and most deprived areas. He stressed the importance of integration, especially as more people are living with multiple, complex health needs.
Speakers shared powerful examples of progress across the city:
- Jim Lovett (Nottingham City East PCN) and Nic Williams (The Renewal Trust) described how regular community hubs in Nottingham City East are successfully reaching diverse groups through thoughtful scheduling, using the right venues and joining up initiatives e.g. inviting asylum seeker and refugee families to receive ‘Feel Good’ packs while introducing them to other organisations that could offer support and advice.
- Lorna Mackie (Raleigh PCN) and Shanine Fasasi (Diversify Education) reminded us that only 20% of health outcomes are driven by healthcare – the rest comes from wider determinants of health. As a result, the PCN and Beechdale Community Centre are on the beginning of their journey of coming together to support marginalised communities and thinking beyond engaging with patients solely through general practice.
- Mark Salisbury (Bulwell & Top Valley PCN) and Natalie Barnaby (CityCare) showcased the achievements that have taken place locally, such as outreach work in local supermarkets, developing local videos and a peer support network to help diabetic patients, health promotion at Bulwell Market and raising aspirations through career fairs at local schools.
The reflections from Nicole Atkinson (CityCare), Patricia O’Connell, and John Burgin (Adult Social Care Team in Nottingham City Council), praised the energy and collaboration shown throughout the day. They reinforced the shared goal of the importance of neighbourhood health, specifically around creating Integrated Neighbourhood Teams, to support patients to receive more coordinated care and telling their stories once.
The event concluded with dynamic discussions around how we could support frail people in Nottingham City through integrated care. Outputs from the event will be used to support the development of a future Integrated Neighbourhood Teams model.
Thank you to everyone who joined – your passion and innovation are vital in tackling health inequality and building healthier communities.
Thank you to everyone who attended, showing such great engagement and willingness to make lives better for the people in their communities. In times where services and resources are stretched so thin, this passion for finding new solutions has never been more important.


